Interview: Daniel P. Sulmasy on informed consent
In an exclusive BioEdge interview, presidential advisor and renown bioethicist Daniel P. Sulmasy discusses the principle of informed consent.

Daniel P. Sulmasy is the Kilbride-Clinton Professor of Medicine and Ethics in the Department of Medicine and Divinity School at the University of Chicago, where he serves as Associate Director of the MacLean Center for Clinical Medical Ethics and as Director of the Program on Medicine and Religion. He is also a member of the Presidential Commission for the Study of Bioethical Issues (PCSBI). Professor Sulmasy has written numerous books on topics related to bioethics, and published many articles in bioethics and medical ethics journals.
In this exclusive interview with BioEdge, Professor Sulmasy shared his thoughts on the complex notion of informed consent.
******
Xavier Symons: Some academics deride the ‘fetishization’ of informed consent or the ‘cult of consent’. What’s going on? Most of us see it as our greatest safeguard.
I understand the sentiment, but informed consent is still critically important. Informed consent has become bureaucratized and, unfortunately, therefore equated by many health care professionals with merely obtaining a signature on a form. Too few practitioners take consent to be a process and a serious moral obligation.
While this can also be true in the research setting, I also think too many ethicists and researchers view informed consent as a sufficient justification for enrolling in human experimentation, and that is also misguided. Some experiments are just too risky or too scientifically flawed to justify doing them even if subjects do consent. These days, patients need more than ever to be involved in their care. The informed consent process is the entrée to their involvement.

XS: You have argued that “free choice is the context of morality, not the content of morality”. Don’t most doctors disagree with you?
I think, sadly, most would not understand what I mean by that statement, and were I to explain, I think they so would have internalized “respect for autonomy” as a principle that they would need to listen to me for a long time to be persuaded that I am correct. As Aristotle puts it, ethics is about what to do, when what to do is up to us.
The goal of ethics is not to increase people’s choices. Rather, ethics concerns the quality of the choices that people freely make. While we ought not to unduly limit people’s freedom, ethics ought to help people to use their freedom to make good choices. So, we ought not merely to be giving patients lists of medical options like a menu in a restaurant.
We ought to help them to make good choices, and that includes permitting physicians to make recommendations based on their experience and practical wisdom. Patients can freely decline the physician’s recommendation, but they deserve guidance to help them to make the best choices that they can make.
XS: Can’t limits on informed consent be seen as a subtle paternalism?
This depends on what those limits are. Some limits on patient choice are justified and the ethical question ought to be whether patients are free to demand from the health care system whatever they choose. For example, I defend a narrow standard of biomedical futility, based on the judgment that a treatment will not work or that the patient will die soon even if the treatment is given.
Under such conditions, one does not, in my view, need informed consent from the patient or family not to provide requested interventions. This is based on the principle that there can be no moral obligation to do what cannot work, and can only result in harm to the patient. This is just common sense ethics, not paternalism. Judgments based on broader understandings of futility, by contrast, can be paternalistic. For example, if the doctor determines that a treatment might work but the quality of life expected for the patient would be too low to justify it even if the family is requesting it, that judgment would be paternalistic and, in my view, unjustified.
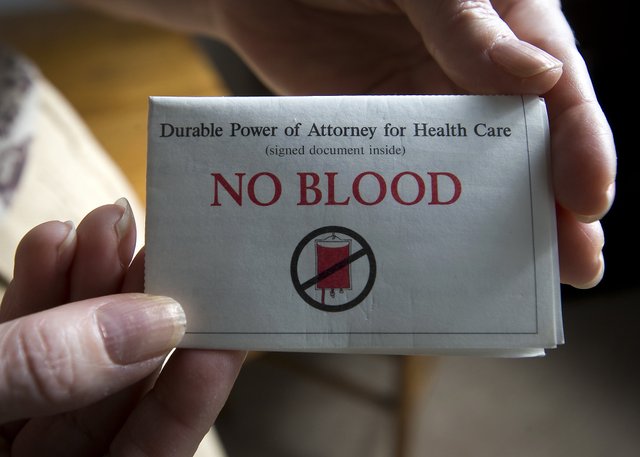
XS: Recently BioEdge reported the case of a pregnant Australian woman who refused a blood transfusion on religious grounds and died along with her baby. How would you have navigated this tragic situation?
This is truly tragic. The sort of case you describe might, for instance, involve a Jehovah’s Witness who holds a religious belief that blood transfusion is gravely sinful. As a general rule, under US law, patients can refuse any treatment for themselves. Nonetheless, also as a general rule, parents are precluded from “martyring” their children. That is, they cannot refuse life-saving medical care for their children on the basis of their own religious beliefs.
Such legal protections, however, only kick in at birth. Until that time, the mother’s right to refuse treatment trumps the effect of that refusal on her developing fetus. For instance, the US Supreme Court banned one city’s policy of incarcerating pregnant cocaine addicts to protect the fetus from the adverse effects of cocaine. So, in the case you describe, one could plead on moral grounds with such a patient on behalf of the not yet born child, but could not transfuse her, legally, against her wishes.
XS: The Grey Matters report from the President’s bioethics commission suggested that patients with impaired consent capacity be included in neuroscience research. How is this consistent with protecting the disadvantaged?
Some medical conditions that are poorly understood and urgently need more research impair the capacity of those who suffer from them to consent to research, making research difficult or impossible to carry out. These conditions are typically neurological afflictions such as Alzheimer disease. People suffering from dementia, for instance, constitute a very vulnerable population, and they deserve protection from exploitation.
Yet a total ban on enrolling such persons in research studies would be short-sighted. The Commission recommends cautious use of surrogate decision makers (such as family members) to give consent for enrolling such patients in a limited set of studies that either hold promise as potential therapies or advance our understanding of the disease from which they suffer. There would need to be safeguards—limits on such surrogate consent—but not an outright ban.
For example, patients with impaired cognition could not be enrolled as subjects in studies about other diseases from which they did not suffer, as this would treat them as mere means of benefiting others. There would also need to be stricter limits on the level of risk that surrogates could consent to permit their loved ones to undertake in such research compared with the risk that a patient with intact decisional capacity might be allowed to take on. Patient assent would be required even if they cannot actively consent (i.e., refusals by patients who are cognitively impaired ought to be respected).
And there needs to be a harmonization of the patchwork of regulations across jurisdictions in the US (and internationally) that set different and often conflicting standards for surrogate consent. We believe reasonable persons would agree to permit such a system, and to have such rules applied to them, were they anticipating the possibility that they might one day become cognitively impaired.
Daniel Sulmasy unpacks the concept of informed consent
Xavier Symons
https://www.bioedge.org/images/2008images/TH_informed_consent.jpg
Creative commons
autonomy
informed consent
interviews
Jehovah’s Witness
virtue ethics
- Can machines be moral? - March 7, 2021
- Can we synthesise Christianity moral theology with secular bioethics? - November 28, 2020
- Euthanasia polling data may fail to capture people’s considered views - August 15, 2020
